Abstract
Background Peripheral artery disease (PAD) is endemic in our globally aging population with >200 million affected worldwide. Graft/stent thrombosis after revascularization is common and frequently results in amputation, major adverse cardiovascular events, and cardiovascular mortality. Optimizing medications to decrease thrombosis is of paramount importance, however limited guidance exists on how to utilize and monitor therapy in this heterogeneous population.
Thromboelastography with Platelet Mapping (TEG-PM) provides comprehensive coagulation metrics and may be integral to the next stage of patient-centered thrombophrophylaxis. This prospective study aimed to determine if TEG-PM could predict subacute graft/stent thrombosis following lower extremity revascularization and if objective cut-point values could be established that were associated with graft thrombosis.
Methods We conducted a single-center prospective observational study on patients undoing lower extremity revascularization within the vascular surgery department. Patients were enrolled over a two year period between December 2020-May 2022, underwent preoperative and serial postoperative TEG-PM analysis at 10 timepoints (pre, peri, post operative), and were followed for up to one year. The primary outcome was a composite endpoint of graft/stent thrombosis requiring reintervention or amputation. Cox proportional hazards (PH) regression analysis examined the association of thrombosis and TEG-PM metrics. Cut-point analysis explored the predictive capacity of TEG-PM metrics for thrombosis and were based on the Youden index.
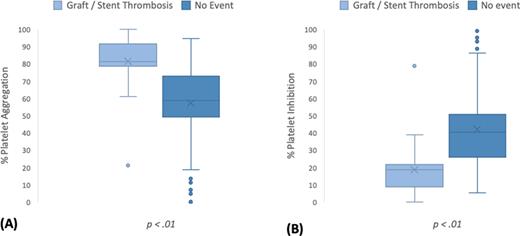
Results A total of 144 patients were analyzed, of which 29 (20.1%) experienced graft/stent thrombosis. Patients who developed thrombosis had statistically greater % platelet aggregation [80.6±15.1 vs. 58.9±25.3] and statistically lower % platelet inhibition [19.8±15.0 vs. 40.8±25.4] (all p<0.01) compared to those who did not (Figure1). Cox PH analysis revealed that for every 1% increase in platelet aggregation, the hazard of experiencing an event during the study period increased by 5% [HR= 1.05, 95% CI 1.03-1.08, p<0.01]. An optimal cut-point of >70.8% platelet aggregation or <29.2% platelet inhibition identifies those at high risk of thrombosis with 90.0% sensitivity.
Disclosures
Dua:Haemonetics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal